Difference Between Fibrosis and Cirrhosis
Key Difference – Fibrosis vs Cirrhosis
The formation of fibrous tissues in any place of our body is called fibrosis. A pathological condition that is marked by the transformation of the entire liver into parenchymal nodules surrounded by fibrous bands and variable degrees of vascular shunting is identified as cirrhosis in clinical medicine. Although the definition of cirrhosis is confusing, if you have a closer look, you will understand that what really happens in cirrhosis is the extensive formation of fibrous tissues in the liver. So cirrhosis is actually a result of the massive fibrosis that takes place in the liver. The key difference between fibrosis and cirrhosis is that fibrosis can happen in any place of the body while cirrhosis is the result of extensive fibrosis taking place in the liver.
CONTENTS
1. Overview and Key Difference
2. What is Fibrosis
3. What is Cirrhosis
4. Similarities Between Fibrosis and Cirrhosis
5. Side by Side Comparison – Fibrosis vs Cirrhosis in Tabular Form
6. Summary
What is Fibrosis?
Fibrosis is the formation of fibrous tissues in any part of the body. Most of the parenchymal organs undergo fibrosis after structural damages to them because of external or internal causes.
Our body uses fibrosis as a mechanism of healing when injured tissues are not capable of complete restitution. It can also happen in tissues that have the potential to regenerate when the supporting structures have suffered irreversible damages. Although these fibrous or scar tissues are not capable of performing physiological functions of the specialized tissues they replace, they provide the much needed structural stability for the intact tissues of the organ to carry out the normal functions.
Causes of Fibrosis
Mechanism of Fibrosis
Following any damage to a parenchymal organ and the subsequent inflammation, a sequential process begins that ends up with the formation of fibrous tissues in the injured organ.
- The process is initiated by the formation of new blood vessels in order to supply blood to the vital factors required for the healing. This is called angiogenesis. The newly formed blood vessels are leaky and this accounts for the edema that is seen around the healing wounds.
Steps in Angiogenesis
- Release of NO and Vascular Endothelial Growth Factors (VEGF)
- Vasodilation
- Separation of the pericytes from the albumin surface and the breakdown of the basement membrane
- Formation of a vessel sprout
- Migration and proliferation of the endothelial cells towards the area of tissue injury
- Remodeling into capillary tubes
- Recruitment of peri-endothelial cells to form mature blood vessels
- Deposition of the basement membrane
- Formation of granulation tissue
Granulation tissue is formed by the migrating and proliferating fibroblasts that get deposited in the loose connective tissues. It has a characteristic pink, soft and granular appearance. The hall mark histological picture of granulation tissues is the presence of tiny blood vessels in an extracellular matrix with interspersed inflammatory cells. TGF-beta is an important growth factor that essential for the successful laying down of the extracellular matrix.
- The last step of the process is the remodeling of the connective tissues.
Remodeling of the connective tissue is extremely important to enhance the stability of the newly formed scar tissue.
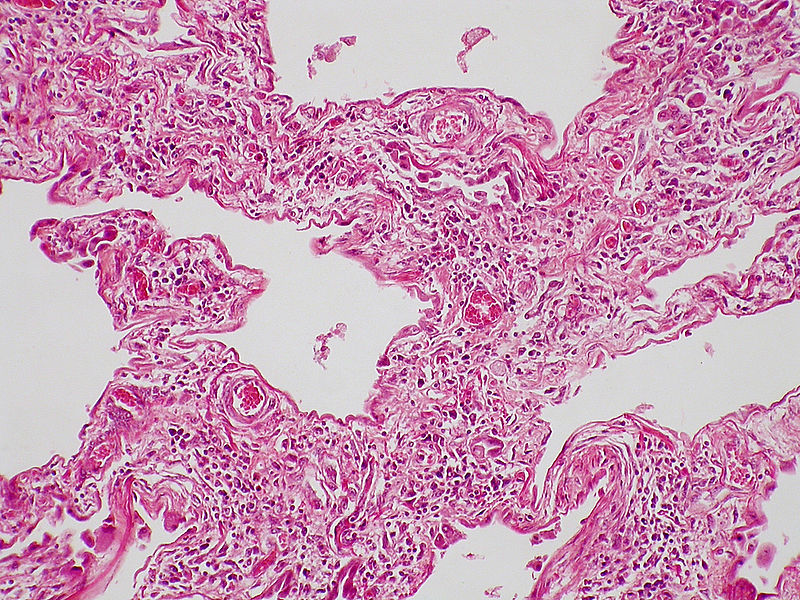
Figure 01: Interstitial pulmonary fibrosis in scleroderma
Macrophages play a key role throughout this process. Major functions performed by the macrophages that assist the healing are,
- Clearing the offending agents and dead tissue
- Providing the growth factors required for the proliferation of cells
- Secreting the cytokines that stimulate the proliferation and migration of fibroblasts
What is Cirrhosis?
Cirrhosis is a pathological condition that is marked by the transformation of the entire liver into parenchymal nodules surrounded by fibrous bands and variable degrees of vascular shunting.
Any condition that gives rise to chronic inflammation of the liver results in extensive destruction of the hepatocytes. Some of the damaged hepatocytes are replaced by viable cells through regeneration and the others are replaced by the scar tissues formed through fibrosis. With repeated exposure to the injurious agent, the destruction of the hepatocytes increases and the number of the cells replaced by fibrosis gradually soar up. The end result of the continuation of this process is the cirrhosis.
Causes of Cirrhosis
- Alcohol
- Chronic viral hepatitis (hepatitis B or C)
- Nonalcoholic fatty liver disease
- Primary sclerosing cholangitis
- Autoimmune liver disease
- Primary and secondary biliary cirrhosis
- Cystic fibrosis
- Hemochromatosis
- Wilson’s disease
- Alpha 1 antitrypsin deficiency
- Any other chronic condition that affects the liver
Pathophysiology of Cirrhosis
Following any damage to the hepatocytes, Kupffer cells and the intact hepatocytes adjacent to the site of injury start to release growth factors and other chemical mediators. These mediators activate the stellate cells in the space of Disse and transform them into mature cells which have myofibroblast like activity. The mature stellate cells then produce mediators that induce the fibrosis.
Morphology of Cirrhosis
- In cirrhosis, the characteristic lobular arrangement of the liver is disturbed.
- As a result of fibrosis, fibrous septae are formed in the liver and they surround clusters of regenerating hepatocytes which are called the regenerative nodules. New blood vessels develop within these fibrous septae and they shunt blood away from the viable hepatocytes.
- Collagen accumulates in the space of Disse.
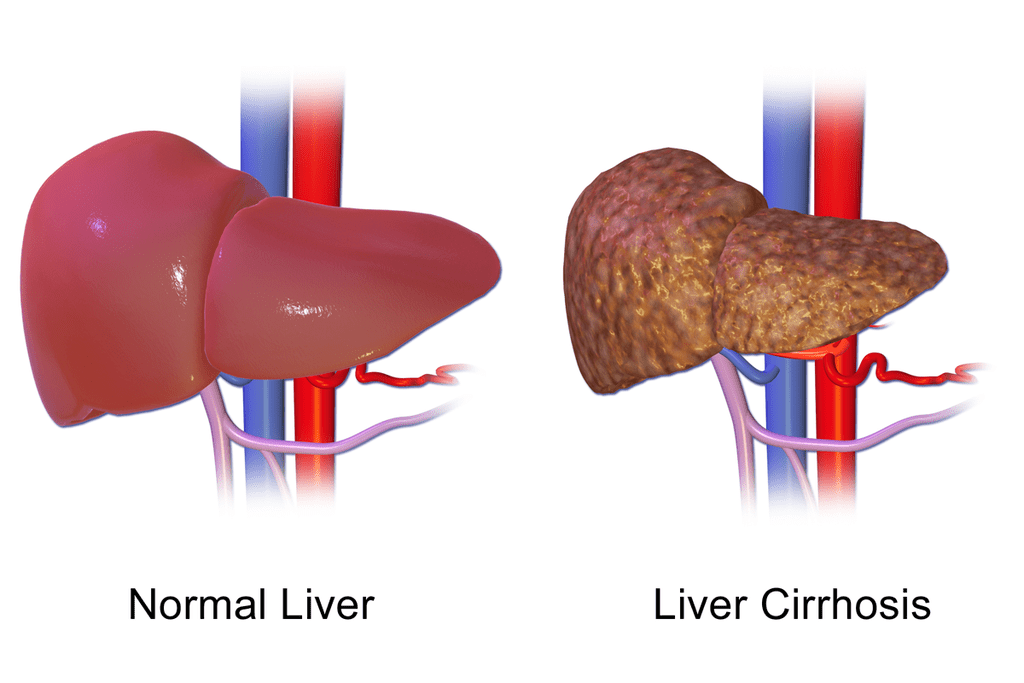
Figure 02: Cirrhosis
Clinical Features of Cirrhosis
- Hepatomegaly
- Ascites
- Jaundice
- Circulatory changes- spider telangiectasia, palmar erythema, cyanosis
- Endocrine changes –Loss of libido, alopecia, gynecomastia, breast atrophy, irregular menses, testicular atrophy, amenorrhea
- Bruises, purpura, epistaxis
- Portal hypertension followed by splenomegaly and variceal bleeding
- Hepatic encephalopathy
- Finger clubbing
In compensated cirrhosis, although the hepatic functions are impaired, they are maintained at lower limits by various compensatory mechanisms. But with the continued destruction of the hepatocytes, these compensatory mechanisms become insufficient. That is when the clinical features start to appear.
Management of Cirrhosis
- Cirrhosis increases the risk of other comorbidities such as esophageal varices and hepatocellular carcinomas.
- Endoscopy should be performed at least once in two years to check for the esophageal varices. Since the clotting factors are not produced adequately by the damaged liver, undiagnosed internal bleeding from the esophageal varices can be fatal.
- Alpha feto protein level of the serum should be measured regularly in a cirrhotic patient to diagnose any malignant conditions in the liver in their preliminary stages.
What are the Similarities Between Fibrosis and Cirrhosis
As discussed at the beginning cirrhosis is just another form of fibrosis. Therefore, both of them have the same pathological basis.
Chronic inflammation is the major cause of both cirrhosis and fibrosis.
What is the Difference Between Fibrosis and Cirrhosis?
Fibrosis vs Cirrhosis | |
| Fibrosis is the formation of fibrous tissues in any part of the body. | Cirrhosis is a pathological condition that is marked by the transformation of the entire liver into parenchymal nodules surrounded by fibrous bands and variable degrees of vascular shunting. |
| Location | |
| Fibrosis can happen in any place of the body | Cirrhosis is the result of extensive fibrosis in the liver. |
Summary – Fibrosis vs Cirrhosis
The severity of fibrosis varies depending on the location where it occurs. For example, the formation of a scar on the skin is nothing to worry about, but the fibrosis in vital organs such as kidneys, liver or lungs can become immensely serious conditions. Cirrhosis is one such occasion where inadvertent fibrosis threatens the life of the patient. This is the difference between fibrosis and cirrhosis. Therefore the early diagnosis of these conditions is important to prevent any future complications.
Download PDF Version of Fibrosis vs Cirrhosis
You can download PDF version of this article and use it for offline purposes as per citation note. Please download PDF version here Difference Between Fibrosis and Cirrhosis.
Reference:
1. Kumar, Vinay, Stanley Leonard Robbins, Ramzi S. Cotran, Abul K. Abbas, and Nelson Fausto. Robbins and Cotran pathologic basis of disease. 9th ed. Philadelphia, Pa: Elsevier Saunders, 2010. Print.
2. Colledge, Nicki R, Brian R. Walker, Stuart Ralston, and Stanley Davidson. Davidson’s Principles and Practice of Medicine. Edinburgh: Churchill Livingstone/Elsevier, 2014 Print.
Image Courtesy:
1. “Scleroderma – Interstitial fibrosis 2” By Yale Rosen – (CC BY-SA 2.0) via Commons Wikimedia
2. “Liver Cirrhosis” By BruceBlaus – Own work (CC BY-SA 4.0) via Commons Wikimedia
ncG1vNJzZmivp6x7pbXFn5yrnZ6YsqOx07CcnqZemLyue8OinZ%2Bdopq7pLGMm5ytr5Wau26yyJupqKuZqHqiusNmraxlk56%2Fs7TOrKCsZw%3D%3D